What to Do When a Loved One Says ‘I Don’t Want to Live Anymore’

What to Do When a Loved One Says ‘I Don’t Want to Live Anymore’
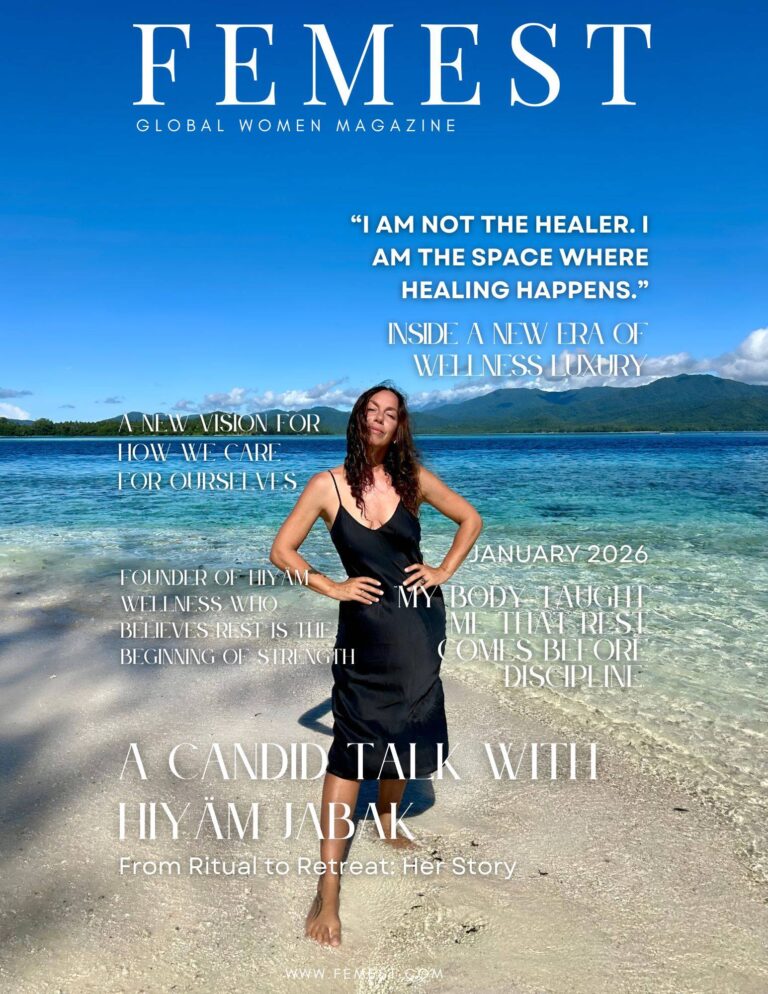
Hearing a loved one say, “I don’t want to live anymore,” can be alarming. Does it mean they’re contemplating suicide? Should you take them to a psychologist immediately? Should you brush it off as a joke or try to help solve their problems? Or perhaps it’s just empty words? Victoria Pravlutskaya, a psychotherapist at the Minsk City Clinical Center for Psychiatry and Psychotherapy, provides insights.
What Leads to Suicide?
Suicidal behavior can manifest as fantasies, thoughts, or actions aimed at self-harm or self-destruction. However, having suicidal tendencies does not always result in suicide. For someone to commit suicide, certain conditions must be met: a combination of various “base” risk factors and “trigger” factors (crisis situations).
Risk Factors
Base risk factors include social, demographic, religious, ethnic, psychological, family, and biological aspects. For instance, men commit suicide more often than women; people over 40 are more likely to commit suicide than younger individuals; those suffering from illnesses and addictions are at higher risk than healthy people. Based on these factors, groups at risk of suicide can be identified, such as “men over 45,” “people with alcohol dependence,” “HIV-infected individuals,” “those with cancer,” and others.
Belonging to a risk group does not guarantee that suicide will occur. However, the probability significantly increases when multiple risk factors are combined. For example, “a man over 45 living alone, suffering from recurrent depressive disorder and alcohol dependence.”
However, a trigger factor is needed to initiate suicidal actions. This is usually a conflict or crisis, often caused by the loss (or potential loss) of a significant person, material or spiritual value. Examples include the death of a loved one, divorce, job loss, loss of health, diagnosis of a serious illness, social and physical helplessness, loss of psychological safety (psychosis, depression), and more.
The presence of such a “trigger” does not necessarily mean that suicide will occur. Whether it happens depends on the strength of the trigger and the number of base factors converging at one point. Interpersonal conflict situations can evoke emotions of fear, guilt, shame, and depression, which often underlie suicidal motivations. If this state is perceived through the lens of helplessness, hopelessness, and the impossibility of an alternative solution, the risk of suicide becomes high. Suicidal perception of the situation is also characterized by cognitive narrowing (“there is no other way out”) and dichotomous thinking (“all or nothing”).
Risk Factors
Socio-Demographic Risk Factors for Suicide
- Gender: The suicide rate among men is 3-6 times higher than among women. The rate of suicide attempts is slightly higher among women.
- Age: The suicide rate in the population increases with age, reaching a maximum after 45 years. The peak of suicide attempts occurs in young people aged 20-29.
- Marital Status: The suicide rate is higher among those who are not married, divorced, widowed, childless, and living alone.
- Professional Status: Disruption of professional stereotypes (job loss, retirement, unemployment status) is associated with an increased risk of suicide.
- Religion: Suicide rates are higher among atheists compared to believers. Among major religions, the highest suicide rates are registered among Buddhists, and the lowest among Muslims; Christians and Hindus are in intermediate positions.
Medical Risk Factors for Suicide
Mental disorders are a serious risk factor for suicide. According to WHO research (2002), in many cases, the person’s condition at the time of suicide meets the criteria for diagnosing a mental disorder. The most common are mood disorders, personality disorders, dependence on psychoactive substances, schizophrenia, and other psychoses. In 31-44% of suicide cases, experts diagnose more than one psychiatric disorder, meaning that comorbidity of disorders significantly increases the risk of suicide.
- Depression: According to some researchers, a moderate or severe depressive episode precedes 45-70% of suicides. The risk of suicide among patients with depression is very high, ranging from 8-30%.
- Alcohol Dependence Syndrome: Between 10 and 22% of those who die by suicide suffer from alcohol dependence. Suicide rates among those dependent on alcohol reach 270 per 100,000, which is almost 20 times higher than the general population (14-17 per 100,000).
- Opioid Dependence Syndrome: The suicide rate among heroin addicts significantly exceeds the general population and ranges from 82-350 per 100,000.
- Schizophrenia: The suicide rate in this group of patients is almost the same as among those suffering from depression, at 10-12%.
- Personality Disorders: The maximum risk of suicidal behavior (3-9%) is associated with emotionally unstable personality disorder, characterized by rapid mood swings, tense interpersonal relationships, impulsivity, feelings of “emptiness” and “meaninglessness,” and black-and-white thinking.
- Other Mental Disorders: High suicidal risk can be associated with disorders such as anorexia nervosa, panic disorder, stress-related disorders, and others. A mental disorder can manifest or be masked by somatic symptoms (autonomic instability, functional gastrointestinal disorders, migraine-like headaches, which can be symptoms of anxiety disorders, somatized disorders, or depression). A mental disorder can also be a consequence of a somatic disease (reactive depression in a patient who has learned about the presence of an incurable disease; anxiety related to the expectation of a serious operation; panic attacks during angina attacks, etc.).
- Somatic Pathology: According to research, about 70% of people who commit suicide suffer from an acute or chronic illness at the time of death. About 50% of this group suffer from a combination of mental disorder and somatic disease.
A group at increased suicidal risk includes patients with severe chronic diseases. In addition to physical suffering or chronic pain syndrome, these diseases bring a lot of negative socio-psychological consequences for the patient. Therefore, somatic diseases often coexist with depression or are one of its causes. The most common conditions leading to suicide include epilepsy; oncological and blood diseases; cardiovascular diseases (ischemic heart disease); respiratory diseases (asthma, tuberculosis); congenital and acquired deformities; loss of physiological functions; HIV infection; conditions after severe operations and transplantation of donor organs and tissues; among patients with other conditions.