Ensuring a Healthy Start: Key Diagnostics for Fetal Development Risks

Ensuring a Healthy Start: Key Diagnostics for Fetal Development Risks
Every expectant mother naturally desires to create a positive environment and avoid adverse factors that could affect her pregnancy. To understand how to identify fetal development pathologies early and what preventative measures are necessary to mitigate risks, we consulted with Galina Kuznetsova, a prenatal ultrasound diagnostics specialist at the EVACLINIC Women’s Health Clinic, and Tatyana Plevako, a geneticist at the EVACLINIC IVF Reproduction and Genetics Clinic.
Galina Kuznetsova
Identifying Fetal Development Risks
Parents can learn about potential developmental issues in their future child through several methods. Firstly, before pregnancy, prospective mothers and fathers can consult a geneticist. The geneticist will collect a medical history and inquire about family health issues. Following this, genetic testing can be recommended to determine if either parent carries any pathological genes. Secondly, once pregnant, a woman should visit her doctor to confirm a normal uterine pregnancy and, between the 11th and 13th weeks, undergo a first-trimester ultrasound screening. This screening checks for indirect markers of chromosomal pathologies and excludes developmental defects.
A non-invasive prenatal test can also be performed, which involves taking a blood sample from the mother to isolate fetal DNA and assess the risk of chromosomal abnormalities. Invasive prenatal tests, such as amniocentesis and chorionic villus sampling, are additional options.
Diagnostics at Different Stages of Pregnancy
Different diagnostic procedures are used at various stages of pregnancy to detect chromosomal abnormalities. Chorionic villus sampling is performed between the 10th and 12th weeks, involving the extraction of a small piece of chorionic tissue to determine the fetal chromosomal makeup. Amniocentesis, which involves collecting amniotic fluid, is conducted from the 16th week to assess the baby’s chromosomal status. Cordocentesis, which involves taking blood from the umbilical cord, is used to confirm or refute a diagnosis when amniocentesis results are inconclusive or to evaluate hematological indicators in cases of Rh conflict.
There is also the Non-Invasive Prenatal Testing (NIPT), a non-invasive procedure where fetal DNA is isolated from the mother’s venous blood for analysis.
Critical Timing for Diagnosing Pathologies
The timing of pregnancy is crucial for diagnosing pathologies. Medically indicated pregnancy termination can only be performed up to 22 weeks. Therefore, it is essential to conduct all possible diagnostics before this period to identify any pathologies and determine their compatibility with the child’s life and potential impact on quality of life. The family makes the decision regarding termination in such cases.
Pathologies Leading to Early Termination
Not all identified defects in the early stages lead to pregnancy termination. It is important to understand whether the defect affects a single organ or multiple organs and how it will impact the child’s quality of life. Families are informed about possible outcomes and offered options such as fetal surgery to correct the defect during pregnancy or surgical treatment during the newborn period.
Avoiding Risks When Preparing for Pregnancy
Proper preparation is key to avoiding risks when planning a pregnancy. Firstly, it is important to determine if the parents carry any pathological genes. If there have been any family health issues, consulting a geneticist and creating a genetic profile is advisable. Additionally, it is crucial to check for folate metabolism disorders, as folate deficiency can lead to neural tube defects and central nervous system developmental issues in the fetus. Women should also be screened for hereditary thrombophilia, which can cause developmental problems in the baby. Many pathologies can be identified through timely fetal diagnostics. Therefore, it is important to register for prenatal care early, follow medical advice, and adhere to all recommendations. Healthy mothers should consult a gynecologist for pregnancy planning to ensure the birth of a healthy baby.
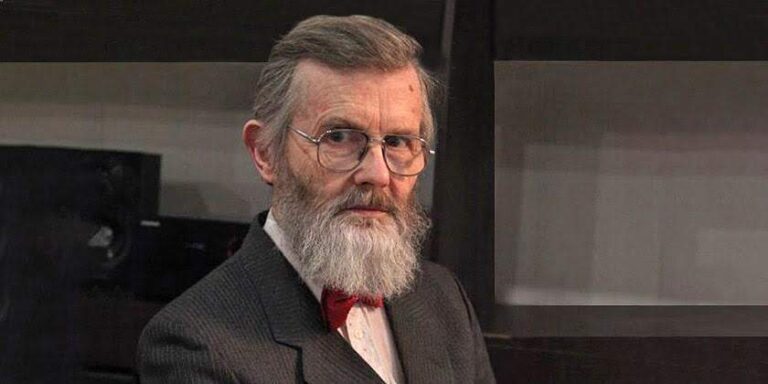
Tatyana Plevako
Identifying Fetal Pathologies at Different Stages
The issue of children born with developmental defects is highly relevant. Prenatal diagnostics, which can identify developmental defects at various stages of pregnancy, is crucial. This allows for informed decisions about further actions. Prenatal diagnostics includes ultrasound and invasive methods. Ultrasound in the first trimester (up to 12 weeks) can detect severe developmental defects, complexes of defects, and markers of chromosomal pathologies. The range of detectable defects is broad, including severe central nervous system defects (such as anencephaly), anterior abdominal wall defects (omphalocele), skeletal dysplasia, and complexes of developmental defects. In the second trimester, ultrasound can identify heart defects, gastrointestinal tract issues, urinary system problems, and other adverse obstetric factors affecting pregnancy.
Invasive diagnostic methods in the first and second trimesters can exclude chromosomal diseases such as Down syndrome, Patau syndrome, and others, as well as monogenic diseases like SMA, Duchenne muscular dystrophy, phenylketonuria, and cystic fibrosis.
Managing Pregnancy with Identified Defects
If a family decides to continue a pregnancy with a fetal developmental defect, they are referred to specialists for more detailed information about the disease, the specifics of managing such a pregnancy, delivery methods, and the availability of specialized medical care. Delivery is planned at a prenatal center with the involvement of pediatricians, geneticists, and specialists to provide timely medical assistance, including surgery if necessary.
Criteria for Early Pregnancy Termination
Several important criteria are considered when deciding on early pregnancy termination:
- Severe diseases or developmental defects
- Untreatable conditions
- Diagnosis confirmed through specific tests
- High genetic risk of an adverse outcome
- Family decision
In the first trimester, up to 12 weeks, pregnancy termination may be considered for genetic reasons if severe developmental defects or complexes affecting multiple systems are identified, if chromosomal diseases are confirmed through genetic testing, or if monogenic diseases are confirmed through DNA diagnostics.
Key Considerations for Planning a Pregnancy
Pregnancy should always be desired and planned. An important step in planning is medical-genetic counseling, which is the most common form of preventing hereditary diseases. The essence of this counseling is to predict the risk of having a child with a hereditary pathology. It is best done before conception or in the very early stages of pregnancy, with the main goal being to prevent the birth of a child with a hereditary disease. Genetic counseling is also conducted in cases of a burdensome hereditary history of one or both parents, consanguinity, exposure to teratogenic factors, and spontaneous abortions.
For more information, you can visit the American College of Obstetricians and Gynecologists.